Options for the young worn knee
This website is a resource for patients and for surgeons and medical professionals to find out about Meniscal Transplantation.
Latest information, rehabilitation programs and centres undertaking the procedure are included in these pages.
To contact a surgeon performing Meniscal transplantation please use the map (CLICK HERE) and link to the surgeons website.
Options for the young worn knee
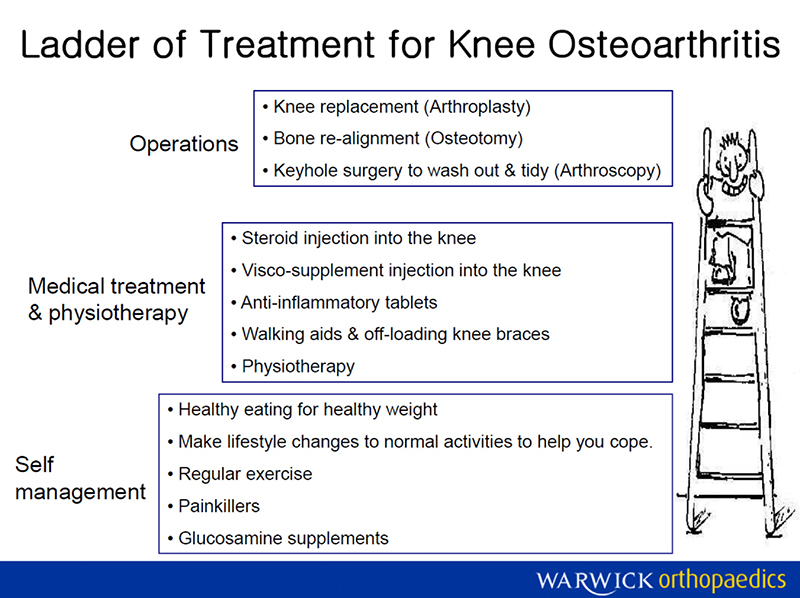
There are various options for treating knee pain caused by wear and tear or injury of the normally smooth joint surfaces. Often there is no single best option and a balanced decision must be made as to what is likely to be best or most appropriate and the options are structured as a ladder of potential treatments. More than one of the treatment possibilities may well need to be considered.
Key points
This information aims to answer questions about what can be done for the
- This information aims to answer questions about what can be done for the worn knee: it can help if you are aware of the options of treatment and how all the options are interlinked.
- It is the overall package of treatment that results in improvement in pain and function.
- It is important to know that some people can have horribly worn looking knees and yet have minimal or no pain at all. Others who have a small worn area in just the wrong place can have substantial symptoms and limitations in what they can do.
- It is possible to have had worn surfaces for a long time before experiencing symptoms of pain and discomfort.
- These pages have been written by Tim Spalding, Specialist Knee Surgeon
The cause of the problem
Excessive sport or an energetic youth is not necessarily the cause of a worn knee. Whilst it is true that football is associated with a higher risk of getting knee damage, marathon runners have no higher risk than anyone else, meaning it is more than just sport that leads to wear. To get joint surface problems, there also needs to be some form of weakness of the joint surface leading to early wear (this is where inherited problems fit in), some form of injury to the joint surface, or an alignment problem in the leg. In other words, joint surface problems can be related to the analogy of having a bad batch of rubber in tyres, taking a divot out of a nice neat lawn or having tyres wear down unevenly because the wheels are out of balance.
The ladder of treatment
The options for treating the worn knee are structured as a ladder and this document details those options and the decision making. The term arthritis is avoided as for most people this conjures up the wrong image and gives the impression of too much doom and gloom. Instead the term wear and tear is used as this more accurately describes the situation.
Surgical techniques and non-surgical management should be combined to achieve the best possible outcome.
NON-SURGICAL OPTIONS
PHYSIOTHERAPY
Physiotherapy aims to improve balance control around the knee and to reduce the sudden forces that go through the joint. The smooth weight-bearing surface in the knee doesn’t mind repetitive low loads but it does mind high impact forces. Muscles work to move the knee but even more importantly their function is to control the shock forces that go through the joint – like creeping down wooden stairs without making a noise or carefully putting a full drink down without spilling it.
Core strength and control is the key, working on the hip and pelvis and buttock muscles to ensure the knee has a good starting point in its movements.
WEIGHT LOSS
If it is imagined carrying a back pack all day filled with 2 – 3 bricks and not taking it off, then it is easy to imagine feeling the strain on the knees. Losing weight is not the easiest thing to do, but knowing that the risk of osteoarthritis is tripled in the overweight person, then it is easy to see how important weight control is, in managing the worn painful knee.
Physiotherapy can help devise a suitable exercise plan to expend energy without upsetting the knee.
VISCO-SUPPLEMENTATION INJECTIONS (SYNVISC or other product)
When the joint is worn the normal lubricant fluid becomes thinner and does not provide the same shock absorbing and lubrication function. The injection boosts the natural lubrication and the benefit can last several months. This seems to work best in patients with mild to moderate arthritis, where probably 60% of patients will notice an improvement. A mild allergic reaction may occur in 2-3% of patients, causing brief increase in pain. This does not seem to affect the result. There are several forms of this injection.
PAINKILLERS
Taking regular painkillers is a simple way of coping with pain from the worn knee. Some people fear the side effects of taking regular medication, but in reality there is only a very low risk from the medication. Regular anti-inflammatory medication such as Ibuprofen (Nurofen, Brufen) or Diclofenac (Voltarol) can upset the stomach and cause ulceration but this is a very low risk. These are usually prescribed by the GP who understands the relevant risks for each individual.
Medications such as regular Paracetamol carry minimal risk and two tablets 2 – 4 times a day can build to give very effective control of symptoms. On top of this there are stronger analgesics such as Tramadol, which can be used for the severe episodes of pain or perhaps taken at night to help with sleeping.
UNLOADING BRACES
When the knee is worn more on one side of the joint than the other, then unloading braces can be used to try and reduce pressure on the affected side of the knee.
Unloading braces work by pushing on one side of the knee to prevent the leg bowing more as weight is taken on it. Braces are useful when the leg is ‘bandy (bow) legged’ or ‘knock-kneed’ and when pain is more on one side of the knee.
Because they work by pushing on the knee, braces can be uncomfortable and some people cannot tolerate wearing them. The brace should only be worn during activities which would normally cause overloading type pain such as prolonged standing at work or undertaking sporting activities. They do not need to be worn when cycling or when around the house.
The picture is one of many styles of brace available.

SURGICAL OPTIONS
There are several surgical options that can be offered to try to improve a joint that is beginning to wear, ranging from a simple keyhole surgery tidy up procedure, through straightening the bowed leg that is overloading one side of the knee, to replacing the lining of the joint using metal and plastic.
ARTHROSCOPY
‘Key hole’ surgery can improve joints where there are mechanical symptoms such as clicking, catching or locking in the knee. During the operation, a small camera is used to look inside the joint and then small instruments are used to remove torn or damaged parts from the knee. During the procedure it is possible to release tight structures or bands of inflamed tissue that could be causing symptoms, or remove build-up of bone that may be blocking movement, or smoothing rough parts of the joint surface. The analogy here is the carpet in a house that is looking a bit thin where an edge has lifted up causing catching. Arthroscopy smoothes down that rough edge, thereby reducing the symptoms – even though the carpet is still worn and looking at bit thin.
Sometimes it is stiffness in the knee joint that causes symptoms of discomfort associated with sitting for prolonged periods or walking. Improving the stiffness can often reduce the level of discomfort. Arthroscopy is generally not of value when the pain is primarily due to overloading and if there are no clicking, catching, or grating symptoms.
OSTEOTOMY OR REALIGNMENT SURGERY
Osteotomy is the surgical procedure for straightening legs, correcting alignment. This is like correcting wheel alignment when the tyres are wearing out unevenly. For the knee this means correcting bowlegged or knock-kneed appearance so the weight is more evenly distributed across the main two compartments of the knee. Ideally the weight bearing axis of the leg, which is a line from the centre of hip to the centre of ankle should pass directly through the middle of the knee distributing the load across both halves. When bowlegged more weight is taken on the inner (medial) compartment of the knee leading to overload pain, and this side is more likely to wear out. Osteotomy for the bowleg is achieved by cutting through the upper part of the shin bone just below the knee, correcting the position under x-ray control and then holding the new position with a plate and screws. Crutches are needed for the first six weeks or so while the bone heals, then gradual return to activity takes place as the bone strengthens. The total downtime before getting back to any impact activity can be up to six months.
Realigning the knock-kneed leg involves an operation on the thigh bone side of the knee joint, again holding it with a plate and screws before allowing full weight on the leg at six weeks.
Overall osteotomy is recommended for patients under the age of 60 who are keen on undertaking energetic activities. Patients must be prepared to endure the rather long recovery period and should understand the purpose of investing in the effort in order to buy time before possibly undergoing knee replacement. The operation is not ideal in patients who have significant restriction in their knee movement or who are substantially overweight, as in these situations the operation unfortunately simply does not improve function or buy any time.
Articular cartilage repair procedures
In general, when the smooth articulating bearing surface of the thigh bone and shin bone are damaged, then it does not regenerate or repair itself. Once the smooth surface (ARTICULAR CARTILAGE) is lost, it seems the body detects the increased pressure and signals this as pain.
There are however some techniques for repairing the surface by trying to regenerate the normal slippery joint surface but these are usually only effective in small areas of damage and not when the whole knee is worn. Also the techniques rely on the body’s own ability to heal, and that unfortunately reduces with age. This means that when the joint is worn enough to be down to bare bone on both articulating surfaces then these repair techniques are not really going to help. Effectively we are talking about trying to re-grow the weight-bearing surface known as articular cartilage, not the footballers cartilage or meniscus as it is properly termed.
There are two main ways to do this. One is stimulating the knee to produce a repair surface with or without a patch to cover it, and the other is to try and grow a new surface in the laboratory from the knee’s own cells and then to reattach it. The techniques are described below.
Microfracture
This is where small holes are made in the worn surface, allowing healthy cells (stem cells) from the underlying bone marrow to regenerate a smooth bearing surface. This is like raking a worn lawn down to a healthy base and hoping new grass grows. Such surgery is usually indicated for the smaller areas of damage but it can be used in larger areas. Often the area is covered by a membrane to contain the new growing tissue.
Autologous Chondrocyte Implantation
This technique grows tissue from the knees own cells – known as chondrocytes – and involves two operations. The first is to take a sample of healthy articular cartilage at arthroscopy. This is then grown in the laboratory into a new tissue which is inserted at a second open operation. There are several methods for this and surgery is usually performed as part of ongoing studies. Recovery time is long while the new tissue matures over 1 – 2 years.
NICE have recently re-approved this after prolonged and somewhat frustrating analysis of cost effectiveness. New techniques are now likely to emerge but these will be restricted to specialist centres.
Limitations of cartilage repair surgery
The aim of cartilage repair surgery is to try and re-grow the normal articulating surface. Unfortunately the body is not good at healing this surface and it is very difficult to get back to a high level of impact type sporting activity such as full contact football or high impact running sports. This means that cartilage repair surgery is less reliable for the individual who wants to get back to these activities, as the quality of repair may simply not be good enough. The aim of surgery is to get individuals back to work, sedentary activities and possibly light sport. The state of the meniscus (footballers cartilage) is also important and these factors are combined together to lead to a decision.
There is a significant downtime after this surgery as the new tissue has to regrow and commitment is needed to the rehabilitation program; in general sport is not advised for 6-9 months after repair surgery and sometimes 12 months depending on the technique. Again these factors need to be discussed with the surgeon when making the decision.
RECONSTRUCTION OF THE MENISCUS
This website is all about Meniscus Transplant for rebuilding the main cushion in the knee – the meniscus or ‘Footballers cartilage’. This is the protective shim in the knee between bearing articular cartilage surfaces of the thigh bone and shin bone.
When this is removed, either partially or totally, then the pressure on the articular cartilage increases and this can lead to early wear. When the main part of the meniscus has been damaged then rebuilding the meniscus is possible using a meniscus transplant. The technique is arthroscopic and the rehabilitation period lasts several months as the new tissue heals.
The procedure is ideal where there is little in the way of wear on the joint surfaces but is less effective when the joint surfaces are already worn.
BIOLOGICAL RESURFACING PROCEDURES OF THE KNEE
It is possible to combine the procedures that have been described, as the success of each is inpart influenced by other factors affecting the knee. For example repairing the surfaces will not last if the knee remains out of alignment. Articular cartilage repair is therefore often combined with the osteotomy procedure. The same applies to the rebuilding of the meniscus as the cushioning needs to be protected by reducing the load across the knee. If the knee is unstable due to a ligament injury then the ligament needs to be reconstructed in addition to rebuilding the joint articular cartilage surface.
The combination of procedures has been termed ‘Biological Resurfacing’. Such surgery is by its very nature complex and not indicated for everyone. The downtime and recovery period can be very long and this surgery is only undertaken after extensive discussions with the surgeon.
PRIORITIES OF TREATMENT: The number one priority is the ALIGNMENT of the leg, the second is the STABILITY of the knee involving ligament reconstruction, the third priority is the state of the MENISCUS involving rebuilding if necessary and finally the fourth priority is the articular surface and repair surgery techniques.
KNEE REPLACMENT – KNEE RESURFACING
At the top of the ladder for treatment is knee replacement. More strictly we should describe this as knee resurfacing with metal and plastic, as the operation involves replacing the worn surfaces of the knee with a shaped metal surface on the thigh bone and a plastic surface on the shin bone. Knee replacement options range from resurfacing part of the joint (unicompartmental replacement) through to resurfacing the whole knee joint (total knee replacement). In addition there are now techniques to insert small implants for isolated areas of damage (partial resurfacing).
Indications for Knee Replacement Because knee replacement carries risks and because the end result is a “metal and plastic” articulation rather than a “normal” knee, the procedure is reserved for a significant level of symptoms when the risks are acceptable. Examples of when a knee replacement is indicated include: not being able to walk a mile, pain at night and feeling that life is on hold because of symptoms.
Age is also important. Patients who are over 60 tend to use their knee less and it is expected that the new knee will then last over 20 – 25 years, whereas under 60 the results of knee replacements are less good with approximately 60 – 70% still working well after ten years. Knee replacements tend to loosen if over used and therefore sport or impact type activities such as may occur with heavy manual work should be avoided after surgery. The plastic surface may wear, or the bond between the metal and the bone may loosen requiring the procedure to be redone. Second or third “revision” procedures are all technically possible but the functional results cannot be expected to be as good as first time surgery due to more scarring around the knee causing joint stiffness and tightness.
Recovery and expectations after Knee Replacement
Following knee replacement, hospital stay is generally 4 – 5 days and crutches are used for up to 4-6 weeks. It takes 2 – 3 months to fully get over knee replacement, before swelling has fully settled and ease of movement has returned. Improvement is still better at a year after the operation.
Functionally it is expected patients to be able to play golf, walk 2 or 3 miles or more, walk up and down hills and undertake light sport such as tennis – but certainly not impact sports such as running or football. Some people have described knee replacement as resulting in the knee function of a 70 year old. This probably fairly accurately summarises the expectations and emphasises how it is important to be in sufficient trouble before considering knee replacement.
Generally we can say that, with appropriate pre-surgery discussions, 8 or 9 out of 10 patients are very happy declaring a whole new lease of life. 1 or 2 in 10 will be unhappy due to either persistent significant discomfort, dissatisfaction with their level of activity or occurrence of a major complication such as infection (1%) or major cardiac or stroke type complications (1 to 2%). Having said all that there is no doubt knee replacement is an extremely successful operation when undertaken for the right indications.